The phenomenon of Troponin elevation in heart failure is a regular and significant occurrence due to its powerful correlation with the pathogenesis, diagnostic procedures, and predictive outcomes connected to this health condition. Thanks to the high-sensitivity cardiac Troponin (hs-cTn) testing method, which has superseded traditional assessments, the interpretation of results has taken on a new dimension while presenting additional challenges.
Correlation of Troponin Levels with Acute and Chronic Heart Failure
More often than not, augmented levels of cTn in acute or chronic Troponin elevation in heart failure demonstrate a correlation with myocardial necrosis (Acute Myocardial Infarction or AMI). The confirmation of an AMI diagnosis comes when further criteria, as defined by the fourth Universal Definition of Myocardial Infarction, are met. Any increase in cTn levels that are still below the AMI threshold may indicate acute or chronic injury, depending on the rising or falling trend curve, or stable levels of cTn as evidenced by serial testing.
The best indicator of troponin elevation in heart failure: acute and chronic heart failure with reduced or preserved ejection fraction (EF) reveal that higher levels of cTn represent a prognostic value for unfavorable outcomes.
Factors Causing Troponin Elevation in Heart Failure
the most important factors that causing troponin elevation in heart failure: Various ischemic or non-ischemic factors can result in a transient surge in cTn levels. These include hypertensive crises, tachyarrhythmias, valvular regurgitation, myocarditis, and stroke, which necessitate a differential diagnosis with Acute Coronary Syndrome (ACS).
Mechanisms Behind Troponin Elevation in Heart Failure
the most important mechanisms of troponin elevation in heart failure which can lead to high cTn levels, including myocardial necrosis or coronary thrombosis (type I MI), imbalance between supply with subendocardial ischemia/injury, cardiomyocyte apoptosis, inflammatory cytokines, and neurohormonal changes.
Understanding Troponin Elevation in Heart Failure: Potential Causes
the most important potential causes of troponin elevation in Heart failure (HF) can result from a myriad of factors, culminating in a troponin elevation noted in afflicted patients .
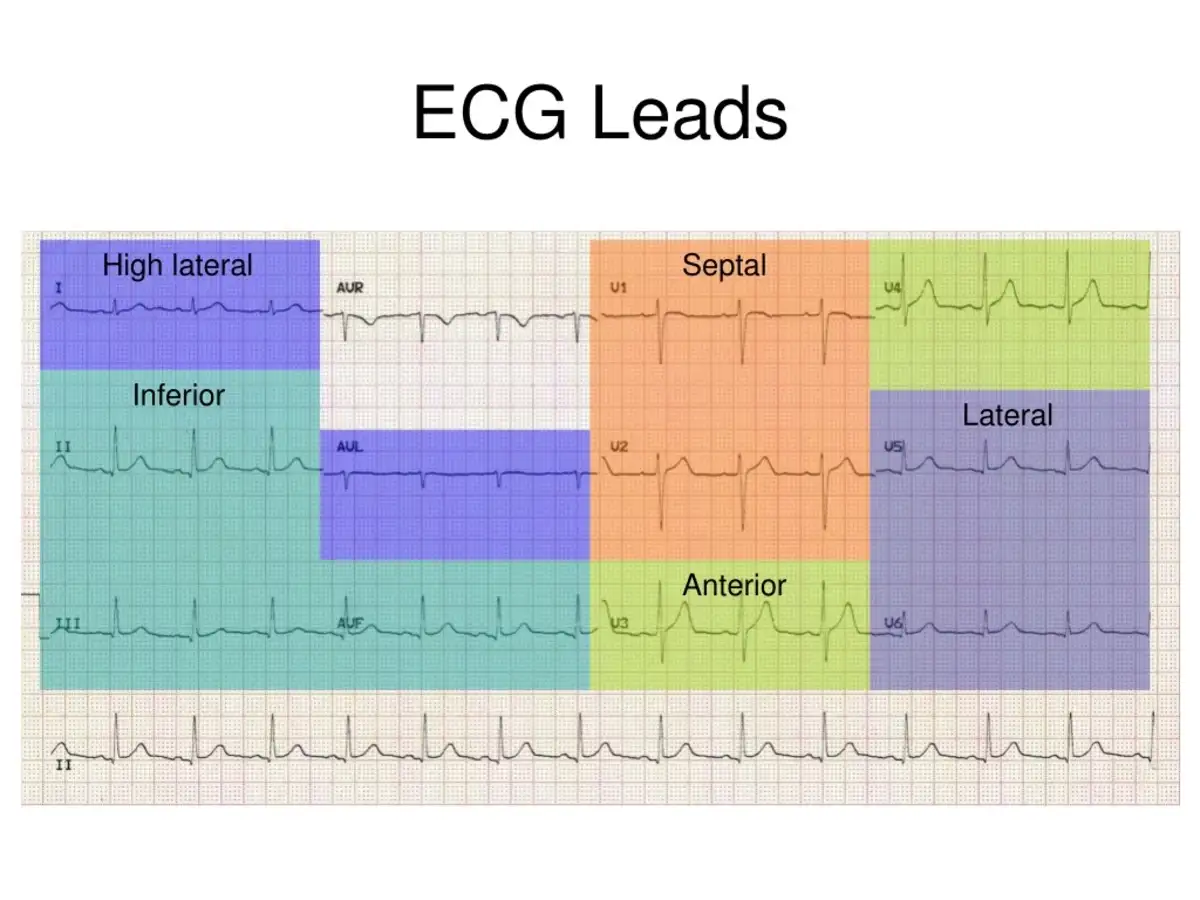
Coronary ischemia is one of the significant triggers for troponin elevation in heart failure, especially through a Type I Myocardial Infarction (MI). This occurs due to issues like atherosclerotic plaque rupture, fissuring, or ulceration. It is crucial to evaluate this, particularly in cases where acute HF syndrome patients show increased troponin levels and signs of acute coronary syndrome, even when classic symptoms may not be readily apparent. Electrocardiography or echocardiography might offer less specificity for patients with historical abnormalities, such as previous MI or underlying left ventricular dysfunction.
In addition to Type I MI, there exists another heart-related factor, Type II MI that can cause troponin elevation in heart failure. This type results from increased transmural pressure, causing a supply-demand imbalance. Patients with HF might also encounter a Type II MI due to small-vessel coronary obstruction, particularly if other indicators of widespread atherosclerosis or diabetes mellitus are present. The prevalence of endothelial dysfunction in HF has considerable potential to cause substantial ischemia and myocardial necrosis. It’s crucial to note that a Type II MI can manifest in the absence of coronary artery disease, potentially due to subendocardial ischemia alone, and is often worsened by lowered oxygen delivery because of prevalent HF-related anemia or hypotension (Figure 4).
Understanding Troponin Elevation in Heart Failure beyond Myocardial Infarctions

While Type I and II MIs explain the substantial troponin elevation in heart failure in both acute and chronic HF syndromes, we must consider other mechanisms. These additional factors releasing troponin in heart failure scenarios are clinically pertinent in many cases. For instance, although troponin release from cardiomyocytes is more commonly associated with MI, it’s not exclusive to this condition. Using highly sensitive troponin testing methods now allows a wide range of values to be measured, implying some level of ‘normal’ cardiomyocyte turnover.
Specific processes, like cardiomyocyte apoptosis and autophagy, tied to wall stretching have been identified through lab trials, revealing these also could increase troponin concentrations. Neurohormones circulating in the body, such as norepinephrine, may lead to direct cellular toxicity and subsequent troponin elevation. Furthermore, heart failure-associated infiltrative processes like amyloidosis have a proven correlation with troponin release and the progressive loss of cardiac functions.
Lastly, troponin elevation may be identified following toxic exposure to substances like alcohol or chemotherapy agents, signaling a risk for potential ventricular dysfunction. Other noteworthy causes of acute HF syndromes, contributing to troponin elevation, include myocarditis and stress cardiomyopathy (also known as Tako-Tsubo cardiomyopathy), mimicking the manifestation of acute MI.
Exploring Non-Cardiac Driven Factors of Troponin Elevation in Heart Failure
Apart from cardiac-centric reasons impacting troponin elevation in heart failure, several other triggers warrant attention when analyzing troponin levels in HF patients. While an array of these factors exists, some stand out for detailed consideration.
A sustained heightened level of troponin above the 99th percentile in HF patients might connect to a slowed clearance of troponin complexes due to inflammatory or autoimmune reactions. The question remains whether this inflammatory response to troponin can expedite the dawn of cardiomyopathy or worsen chronic HF. Additionally, skeletal muscle disease could trigger a significant increase in troponin T levels, this is believed to be linked to the reactivation of fetal gene programs. Instances of abnormal troponin readings in the environment of heterophile antibodies, notwithstanding unapparent cardiovascular dysfunction, have also been reported.
Troponin Elevation in Heart Failure: Profound Impact of Renal Failure
How troponin elevated in heart failure affects the kidneys?
A non-cardiac factor significantly associated with raised or measurable troponin in HF patients is renal failure. The precise cause of troponin release in renal disease sufferers remains vague, however, unmistakably, the troponin source is cardiac. The reliance of troponin I or T on renal function for their clearance is still a mystery. Nevertheless, it is becoming generally accepted that a substantial portion of circulating troponins in chronic kidney disease patients may stem from existing structural heart disease, and/or direct toxic impacts of renal failure on the myocardium, as opposed to affecting troponin clearance. Considering the molecular weight of troponin, clearance should be less reliant on glomerular filtration.
Interestingly, when troponins elevate in patients with renal failure, they prove highly prognostic. A troponin level above the 99th percentile in an HF patient with renal failure should not be hastily dismissed as a ‘false-positive’ due to reduced clearance. While troponin T seems to have a higher chance of being elevated or measurable in renal failure patients compared to troponin I, the advent of highly sensitive troponin testing methods raises the question if this discrepancy will persist in the future.
The Role of Troponin Elevation in Heart Failure Syndromes
the most important role of Troponin Elevation in Heart Failure that A substantial number of patients suffering from acute HF syndromes experience a Type I acute MI as the primary cause. Consequently, recent consensus guidelines emphasize the exclusion of Type I MI during initial evaluations of those suspected of or confirmed with acute HF syndromes. When assessing troponin levels in HF patients, interpretation should align with MI diagnosis guidelines. This requires additional corroborating evidence like a unique increase and/or drop of the marker above the 99th percentile of a standard reference population, changes in electrocardiograms, or imaging evidence of new functional myocardium loss under circumstances typical of coronary ischemia.
Existing data on the utilization of troponin testing in acute HF syndromes offers noteworthy insights (Supplementary Data). Depending on the study, troponin elevation in acute HF syndromes can range from relatively rare to commonplace. As an example, an analysis of over 105,000 patients showed that while 75% displayed detectable troponin, only a small 6.2% had a value above the upper reference limit. Interestingly, troponin levels did not show a distinct association with HF resulting from ischemic heart disease or prevalent acute MI.
Troponin Elevation in Heart Failure and its Prevalence in Acute Syndromes
we talk a bout troponin elevation in heart failure so The frequency of ‘elevated’ troponin in HF syndromes heavily depends on the severity of HF, the cut-off point selected, and the sensitivity of the testing method. For instance, lowering the cut-off to the limit of detection results in a larger number of patients showing measurable troponin values. Reports indicate that using high-sensitivity troponin methods calibrated for use at the troponin 99th percentile (corresponding to the upper reference limit of a healthy population) will allow detection of a higher percentage of elevated results in acute HF contexts.
The common occurrence of measurable or frankly elevated troponin values in acute HF, which may manifest independently of a Type I MI, has consistently been associated with an increased risk of mortality, independently of other risk markers like ventricular function, age, and other biomarkers such as natriuretic peptides (Figure 1). It is likely that highly sensitive troponin tests may enhance our ability to risk stratify above conventional troponin tests when the latter’s concentrations are below their precision range. The value of highly sensitive troponin for prognosis appears especially prominent when it’s measured in a sequential manner, enabling the identification of the highest-risk patients, typically with an increasing pattern.
Read also: Can an echocardiogram detect breast cancer